Couture, C., Zaniolo, K., Carrier, P., Lake, J., Patenaude, J., Germain, L., Guérin, S. (2016) “The tissue-engineered human cornea as a model to study expression of matrix metalloproteinases during corneal wound healing” Biomaterials, Vol.78, 86-101.
Scientific impact: An in vitro model of reconstructed cornea was produced with human corneal keratocyte incorporated into a collagen matrix. Human epithelial cells and bovine endothelial cells were then seeded on the surface. The expression of adherent junction proteins, such as cadherin and catenin (alpha and beta), was observed showing that the model reproduces the polarization and differentiation processes that take place in native cornea. This human corneal model reconstructed in vitro is a promising tool to study mechanisms that regulate normal and pathological conditions related to the cornea.
Network contribution: The Vision Health Research Network has contributed to this work by funding the Ocular Tissue Bank. Indeed, human corneal cells used in this work were obtained from cornea discarded for human transplantation. These cells have allowed us to advance knowledge on the mechanisms underlying differentiation of human corneal epithelial cells and keratocytes. Thereby, the Ocular Tissue Bank gives us the possibility to obtain ocular tissues processed in conditions allowing to preserve cell properties and viability and to permit subsequent in vitro cell culture, this is essential for our research.
* * *
Original Abstract
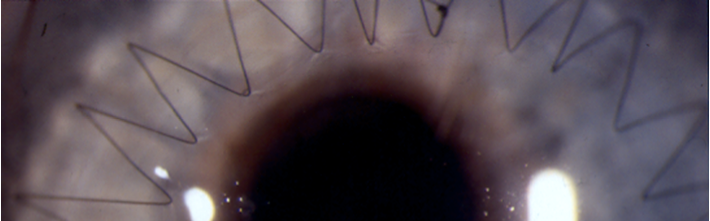
Corneal injuries remain a major cause of consultation in the ophthalmology clinics worldwide. Repair of corneal wounds is a complex mechanism that involves cell death, migration, proliferation, differentiation, and extracellular matrix (ECM) remodeling. In the present study, we used a tissue-engineered, two-layers (epithelium and stroma) human cornea as a biomaterial to study both the cellular and molecular mechanisms of wound healing. Gene profiling on microarrays revealed important alterations in the pattern of genes expressed by tissue-engineered corneas in response to wound healing. Expression of many MMPs-encoding genes was shown by microarray and qPCR analyses to increase in the migrating epithelium of wounded corneas. Many of these enzymes were converted into their enzymatically active form as wound closure proceeded. In addition, expression of MMPs by human corneal epithelial cells (HCECs) was affected both by the stromal fibroblasts and the collagen-enriched ECM they produce. Most of all, results from mass spectrometry analyses provided evidence that a fully stratified epithelium is required for proper synthesis and organization of the ECM on which the epithelial cells adhere. In conclusion, and because of the many characteristics it shares with the native cornea, this human two layers corneal substitute may prove particularly useful to decipher the mechanistic details of corneal wound healing.
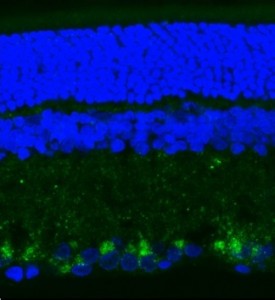
Dual leucine zipper kinase (DLK) immunofluorescence of retinal sections 72 h after optic nerve transection in rats (in blue: DAPI staining, in green: DLK, a key neuroprotective target in retinal ganglion cells).