Giasson CJ, Deschambeault A, Carrier P, Germain L. Adherens Junction Proteins Are Expressed in Corneal Equivalents Produced in Vitro with Human Cells. Mol Vis Molecular Vision. 2014, 20 : 386-394.
Scientific impact: This paper demonstrates that tissue-engineered human corneas are an excellent model to study corneal wound healing. In fact, we have shown that the expression of matrix metalloproteinases occurring during wound healing in our reconstructed cornea is essentially the same that participate during wound healing of native corneas. Because of this similarity between our model and the native cornea, this study suggests that our reconstructed cornea could replace the use of animal model or cadaveric cornea to study corneal wound healing. While the use of animals in research is expensive, and while post-mortem corneas are rare, our reconstructed corneas appear to be a great alternative to those models. They are less costly, devoid of differences between the samples, easily accessible and already applied to humans. This paper has allowed us a better understanding of the mechanisms of corneal wound healing. Beyond the field of vision, our discoveries may also find applications in wound healing of other tissues, such as the skin, because of the many similarities the cornea share with this tissue.
Network contribution: The Vision Health Research Network has contributed to this work by funding the Banque d’yeux du Centre Universitaire d’Ophtalmologie du Québec, from which corneal fibroblasts and epithelial cells are derived to produce the human tissue-engineered corneas. Also, the Graduate Student Performance Award that Camille Couture received during her master degree encouraged her to pursue in the vision research domain, which conducted to the results presented in this article. She is currently PhD graduate student in the vision domain at Université Laval.
* * *
Original Abstract
PURPOSE: To test whether adherens junction proteins are present in the epithelium and the endothelium of corneal equivalents.
METHODS: Corneal cell types were harvested from human eyes and grown separately. Stromal equivalents were constructed by seeding fibroblasts into a collagen gel on which epithelial and endothelial cells were added on each side. Alternatively, bovine endothelial cells were used. At maturity, sections of stromal equivalents were processed for Masson’s trichrome or indirect immunofluorescence using antibodies against pan-, N-, or E-cadherins or α- or β-catenins. Alternatively, stromal equivalents were dissected, to separate the proteins from the epithelium, endothelium, and stroma with sodium dodecyl sulfate-polyacrylamide gel electrophoresis. Western blots of the transferred proteins exposed to these primary antibodies were detected with chemiluminescence. Native corneas were processed similarly.
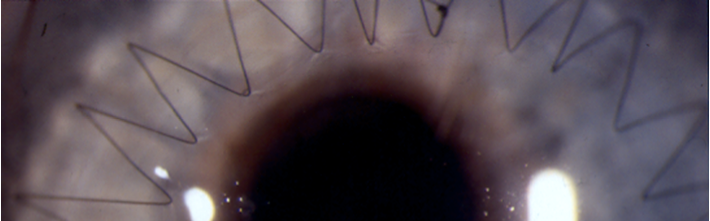
RESULTS: Three or four layers of epithelial cells reminiscent of the native cornea (basal cuboidal and superficial flatter cells) lay over a stromal construct containing fibroblastic cells under which an endothelium is present. Western blots and indirect immunofluorescence revealed that, similarly to the native cornea, the epithelium reacted positively to antibodies against catenins (α and β) and E-cadherin. The endothelium of corneal constructs, whether of human or bovine origin, reacted mildly to catenins and N-cadherin.
CONCLUSIONS: This collagen-based corneal equivalent simulated the native cornea. Cells from the epithelial and endothelial layers expressed adherens junction proteins, indicating the presence of cell-cell contacts and the existence of polarized morphology of these layers over corneal equivalents.
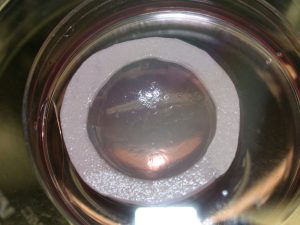
Macroscopic view of a corneal equivalent in its Petri dish after 25 days in culture.